How Remote Therapeutic Monitoring Enhances Decision-Making and Patient Relationships
How Remote Therapeutic Monitoring Enhances Decision-Making and Patient Relationships
Healthcare is changing—fast. One of the biggest shifts we’re seeing isn’t just about patients accessing data, but how clinicians use that data to make sharper decisions, take earlier action, and build stronger relationships with the people they serve.
Remote Therapeutic Monitoring (RTM) is a tool that empowers clinicians with real-time, relevant, and easy-to-understand information that can reshape the entire care experience.
Let’s look at how RTM is giving providers what they’ve needed all along: the clarity, context, and connection to deliver better care—with more confidence.
Beyond the Office Visit: Closing the Gaps in Clinical Visibility
Without ongoing insight between visits, clinicians have traditionally relied on patient self-reporting and adherence. But when follow-ups reveal a lack of progress—or worse, a setback—it’s often too late to make timely adjustments, costing patients valuable recovery time.
Remote Therapeutic Monitoring changes that. With platforms that collect real-time, non-physiologic data—such as mobility patterns, therapy adherence, pain levels, and functional status—clinicians are no longer guessing.They’re tracking real progress continuously and can catch issues before they escalate.
Less Chart Chasing, More Clinical Thinking
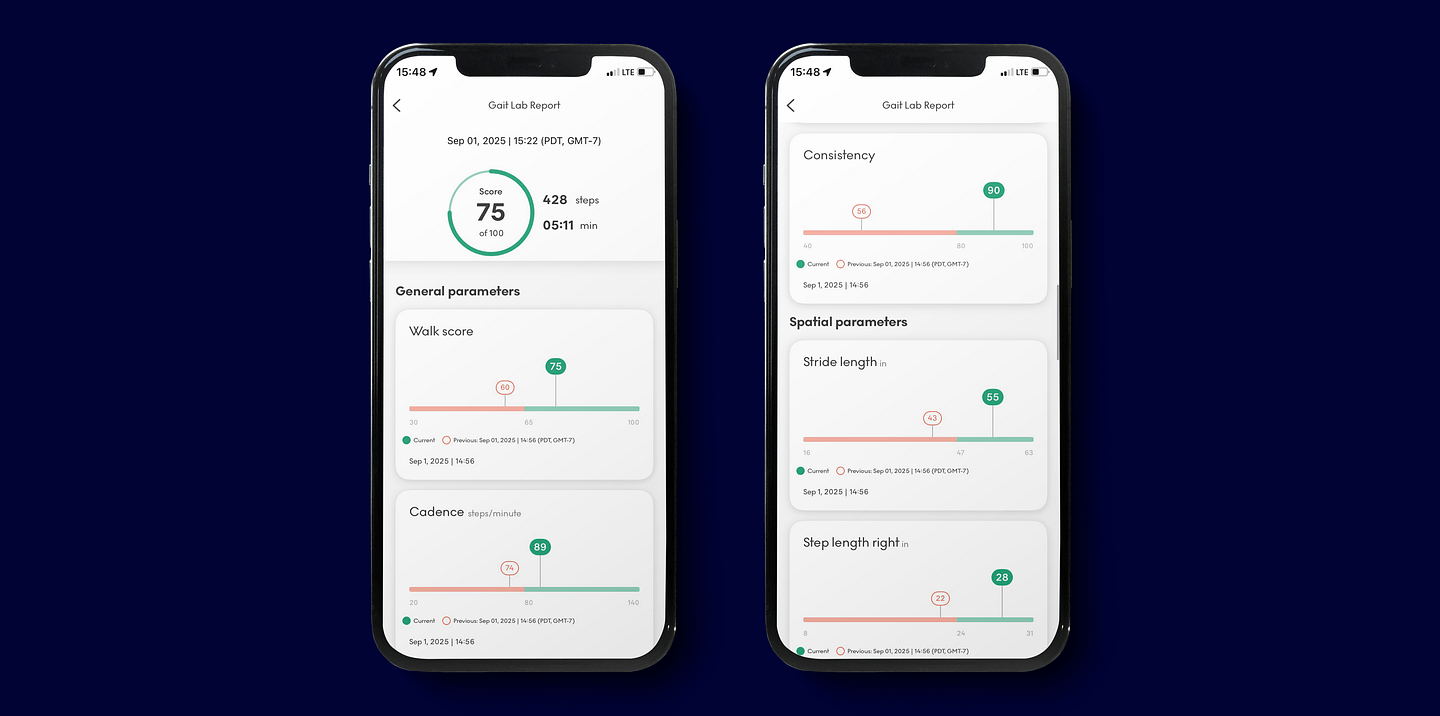
Every provider knows the stress of digging through incomplete charts, trying to piece together a timeline from fragmented data. Remote Therapeutic Monitoring platforms cut through that noise by delivering organized, easy-to-interpret dashboards that highlight trends over time.
Rather than wading through data silos, providers get a clear snapshot of what matters most:
- Changes in gait speed – A decline may indicate pain, fatigue, or the early onset of functional deterioration, prompting timely clinical intervention.
- Balance irregularities – Even subtle shifts can signal increased fall risk or neurological issues that require attention.
- Missed rehab days – Gaps in participation are flagged automatically, helping care teams follow up before progress stalls.
- Mobility progress since last check-in – Clinicians can track gains (or setbacks) in real time, allowing for fast, informed adjustments to care plans.
With that clarity, clinicians can make decisions faster and with greater precision, focusing more on problem-solving and patient strategy—and less on admin work.
Earlier Intervention = Better Outcomes
One of the greatest strengths of Remote Therapeutic Monitoring is the ability to detect subtle changes before they become major problems. A drop in activity, slower walking speed, or deviation in gait pattern may indicate a risk of injury or decline in condition. RTM flags these changes in real time.
This enables early, proactive intervention—adjusting a care plan, reaching out with encouragement, or recommending in-person treatment when needed.
From Data to Dialogue: Building Trust Through Transparency
Patients today want more than check-ins—they want to feel seen and supported. Not only that, they want to see results, and fast. When clinicians reference real-time therapy and mobility trends or point to visible progress on a dashboard, patients often feel more engaged in their own recovery. It turns abstract goals into something attainable.
RTM creates a two-way conversation instead of a top-down directive, changing the entire dynamic. These conversations build rapport, trust, and accountability—strengthening the relationship beyond the exam room.
Making Every Visit Count
With Remote Therapeutic Monitoring, in-person and virtual visits are more productive. Clinicians can walk in prepared, with recent trends and performance already in hand. That means less time is wasted gathering background information and more time is focused on what matters most: progress, planning, and patient goals.
It also reduces patient frustration. There’s no need to “remember how they felt last week” or try to self-report every health concern. The app-based data does the tracking, so patients can focus on healing.
Smart Technology That Learns and Adapts
RTM has evolved. It’s not just about collecting data, but using it to drive smarter, faster clinical decisions. Some platforms use AI to surface insights, prioritize alerts, and suggest areas for attention based on individual baselines.
For providers, this means spending less time scanning for problems and more time responding to the right ones. It’s a smarter workflow that supports clinical intuition with timely, data-driven cues.
And since these platforms are mobile-first and device-free, clinicians and care teams can access insights anywhere—whether they’re rounding at a facility, working from home, or consulting with specialists.
Human Impact: Confidence for Providers, Support for Patients
Ultimately, Remote Therapeutic Monitoring brings something deeper to healthcare—and that is confidence. When providers can see progress and catch red flags early, they feel more in control of outcomes—and patients sense that confidence.
RTM also supports continuity of care across more provider types, including physical therapists, occupational therapists, speech-language pathologists, and psychologists—giving the entire care team shared visibility into the patient’s recovery.
That shared insight reduces miscommunication and aligns everyone around the same goal: better, faster, more personalized care.
RTM Isn’t Just Technology—It’s a Strategy
What makes Remote Therapeutic Monitoring (RTM) so impactful isn’t just the data it gathers—it’s the strategic way that data is used to deliver better care. The most effective RTM platforms aren’t just tools; they are clinical partners designed to support decision-making and strengthen care delivery. Here’s how:
✔ Simplify clinical workflows: RTM platforms automate much of the heavy lifting—from tracking adherence and mobility data to flagging functional setbacks—so clinicians can focus on patient care. Instead of sifting through fragmented data across multiple systems, providers have everything they need in one place, easy to interpret. It’s a game-changer for practices balancing high patient volumes and limited time.
✔ Enable faster, evidence-based decision-making: When real-time data is delivered directly to a clinician’s dashboard, it becomes easier to spot trends, make earlier decisions, and personalize therapy plans. Rather than relying on patient self-reporting, providers access continuous, objective data reflecting functional outcomes.
✔ Strengthen provider-patient relationships: RTM creates new touchpoints between visits, helping patients feel seen and supported through their recovery journey. When providers follow up based on therapy milestones or flag early signs of disengagement, patients feel more connected and more likely to stay on track. That consistency builds trust—and trust builds outcomes.
✔ Encourage early, proactive interventions: By flagging subtle declines in movement quality or therapy adherence before they escalate, RTM helps clinicians intervene earlier. Whether it’s adjusting a therapy plan or scheduling a check-in, small shifts made early can prevent bigger problems later.
✔ Improve outcomes while reducing preventable issues: Ultimately, the goal of RTM is to support healthier, more functional patients. With earlier action and higher adherence, outcomes improve. Whether it’s avoiding a setback, reinforcing recovery progress, or guiding patients through complex rehab, RTM reduces preventable events and supports long-term success.
Empowering Providers to Lead with Clarity and Care
Remote Therapeutic Monitoring is more than a tech upgrade—it’s a clinical advantage. It equips providers with the insights they need to act early, build trust, and lead confidently through every step of the care journey.
For clinicians ready to move beyond reactive care, RTM offers something powerful: a smarter way to treat—and a stronger connection to the people they’re treating. Contact us to learn more!


